The Emotional Impact of Eczema
Reviewed by: HU Medical Review Board | Last reviewed: October 2024 | Last updated: October 2024
Eczema is the world’s leading cause of skin disease. Identified by an itchy red rash, the skin condition can carry a heavy emotional impact. Atopic dermatitis is the most common type of eczema.1-5
Eczema is widespread among children but can continue into or come back during adulthood. A 2023 study found that about 20 percent of all children have atopic dermatitis. Between 7 and 10 percent of adults have the condition.1-3
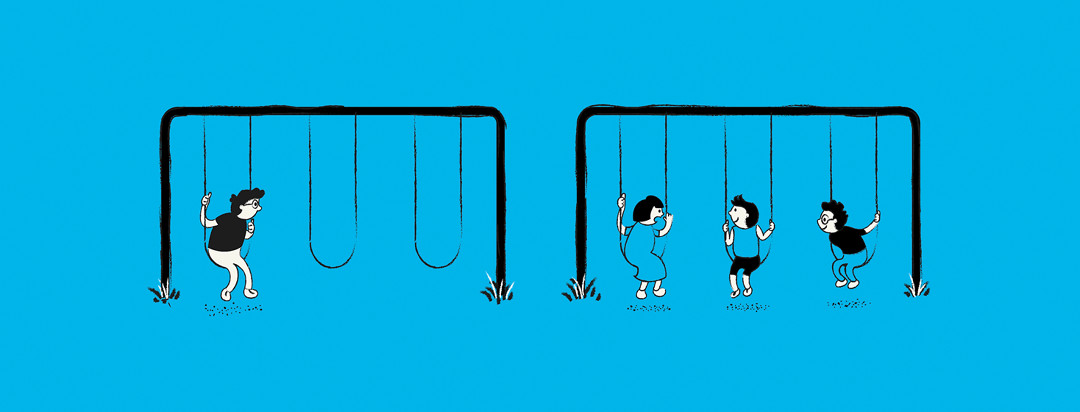
Children with eczema may be teased or bullied by classmates because of the condition. This can lead to emotional isolation and depression. Adults with eczema can also face stigma in their social lives and in the workplace. In a 2024 study, 67 percent of respondents said they faced one or more of the following because of their condition:1-4
- Stigma
- Teasing
- Bullying
- Discrimination
- Low self-esteem
- Withdrawal from others
Eczema and mental health
Both adults and children with eczema have higher rates of stress, anxiety, and depression than their peers without the skin condition. Higher levels of stress can make itching worse and trigger flares. In fact, in 1 study, 57 percent of women and 41 percent of men with atopic dermatitis said that stress was the biggest trigger for skin flare-ups.1-5
Long-term (chronic) stress is more likely than short-term (acute) stress to worsen inflammation in people with eczema. For many people with eczema, their condition itself is a source of chronic stress.2,5
The link between eczema and stress creates a vicious cycle of physical and emotional discomfort. Stress can make the inflammation and the itching worse. But then scratching inflames the skin more and causes more stress. Also, a compulsive need to scratch can add to the stigma that people with eczema face.5
As the condition worsens, people with eczema may become more self-conscious about their skin. This is especially true if the rash is in a visible area, such as the arms, legs, or face. Self-consciousness can increase feelings of depression and a desire to withdraw socially. Children may not want to go to school. Adults may avoid meeting with friends. In the most severe cases, people have reported thoughts of suicide.1-5
The impact of eczema on sleep
Many people living with eczema have intense itching around the inflamed areas. It can be so bad that it leads to sleeping problems. They may wake often during the night and need to scratch to relieve the itching.1-3,5
If this is the case, the result can be another vicious cycle. A lack of quality sleep can lead to tiredness the next day. Children may then have problems focusing at school, affecting their grades. Adults may have trouble completing their work, affecting their job performance. Both of these effects can cause more stress.1-3,5
Seeking help to manage stress
Treatments to manage the rash caused by eczema include topical ointments and exposure to UV light (phototherapy). But many people with eczema may also benefit from seeing a mental health counselor or therapist to help them manage the stress they face.1,2
A therapist can teach them techniques to help them cope with the emotional aspects of the disease. Therapy provides a safe space to talk about the stresses and stigma they may face in daily life. And a therapist can help identify other stressors that may impact emotional well-being. These may include lack of sleep or exposure to certain trigger foods, such as alcohol.1-3,5
Therapists also may use stress-reduction tools to lessen the effect of stress on people living with eczema. Cognitive-behavioral techniques and habit reversal training may help people to recognize and distract themselves from the need to scratch.5
In general, when stress levels begin to rise, deep breathing or progressive relaxation techniques can be useful. Yoga, visualization exercises, and meditation can also help.5
Finally, getting regular exercise can be an effective way to reduce stress. People with eczema who are self-conscious about their skin may shy away from gyms or team sports. However, exercise can benefit both physical and emotional well-being.2,3,5